What is carpal tunnel syndrome?
Why the symptoms are prevalent during the night or when you wake up in the morning?
What are the risk factors of the Carpal tunnel syndrome?
What is the frequency (prevalence) of carpal tunnel syndrome?
How to diagnose a carpal tunnel syndrome?
Does carpal tunnel syndrome get worse progressively?
What is carpal tunnel syndrome?
It’s a set of symptoms due to the compression of a nerve (median nerve) in its passage through an anatomical tunnel, situated between the wrist and the palm, named carpal tunnel. Hence the name Carpal Tunnel Syndrome or CTS.
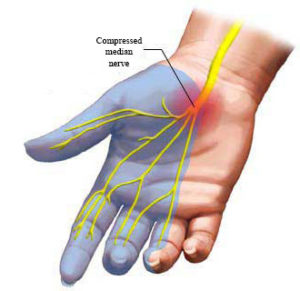
Median nerve (in yellow) compressed at the level of the carpal tunnel (the region between the wrist and the palm).
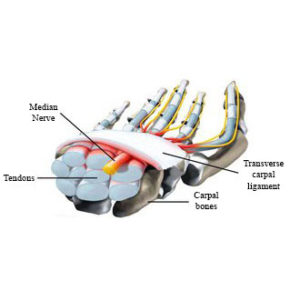
Cross section of the carpal tunnel (median nerve in yellow).
What are CTS symptoms?
- Paresthesia (pins and needles, numbness, tingling sensations) particularly frequent in that part of the hand innervated by the Median Nerve, that is in the zone of the first three/four fingers (thumb, forefinger, middle finger, ring finger) and in the corresponding zone at the palm;
- Wrist and hand pains, but also pains that are radiated or present in the zone of the forearm, arm, up to the shoulder;
NB: Paresthesias and pains are mainly present at night and when you wake up in the morning. - Hypoesthesia (recuced sensibility) on the skin of the first three/four fingers of the hand and on the corresponding part of the palm; it’s manifested by sensations of “sleeping skin” that makes it difficult to recognize by touch the items seize or the necessary strength to keep a proper grip; as a result objects can slip from the fingers;
- Hyposthenia (reduced strength), particularly in some hand muscles situated in the base of the thumb (thenar eminence) and innervated by the Median Nerve.
Why the symptoms are prevalent during the night or when you wake up in the morning?

The rest, especially the night, favors the onset of symptoms.
Basically it’s not clear; some specialists have documented an increasing pressure inside the carpal tunnel during the night, particularly in the first hour of the morning, with consequent compression of the nerve. The causes of this, however, are not entirely clear. Probably the factors responsible of this night compression of the nerve are various. A first important factor is probably the lying position (supine), through a relative redistribution of the body fluids to the upper limbs, with a higher pressure in the carpal tunnel as well. Another important factor could be represented, paradoxically, by the rest of the hand, because of the absence of movement (of the tendons) and consequently the lack of a pump and dreinage action on the intracarpal fluids, which would tend to accumulate. On the other hand it’s common experience of patients to find relief by moving and flapping their hand repeatedly. Other possible reasons could be the flexed finger position that seems to favour the re-entry in the tunnel of some little hand muscles (lumbrical muscles) with consequent higher compression on the median nerve. Lastily, during the night you can remain with the wrist bent or hyperextended with a higher compression on the nerve.
What are the risk factors of the carpal tunnel syndrome?
Risk factors
- Excessive use of the hand in working activities. Particularly in those one that have to deal with exercises against finger resistance, use of tools compressing on the palm or on the wrist, use of vibrating instruments etc.
- Female sex. Because of anatomical reasons regarding the structure and dimension of carpal tunnel but above all for hormonal reasons. Since estrogens have a relieving effect while progesterone have a damaging effect, the syndrome is much more frequent in perimenopausal age or during pregnancy.
- Diabetes or other dysmetabolic or disendocrine disorders (for example renal failure or reduced thyoid functions). Diabetes, a rather frequent condition among people in general, adds damage to the nerve fibers on the mircocirculatory level to the compressive conditions, leading to an increased expression of the syndrome.
- Arthrosis or arthritis, especially of deforming nature on the bones/articulations of the carp, which constitute the basis of carpal tunnel.
- Previous wrist fractures with residual osteoarticular deformity in the carpal zone.
- Genetic predisposition (for example for the family-based shrinkage of the tunnel).
- Other various causes (of rare frequency).
Mechanisms by which risk factors act
- Increase in content of tunnel.
Mainly tendonitis, tenosynovitis and tenidinosis (related to an overuse of hands in woking activities) lead to an enlargement of tendon sheaths inside the tunnel and then to a reduction of the space available for the nerve, that is consequently compressed. The increase in content of the tunnel can be also caused by imbibition of fluids, due to hormonal factors such as during pregnancy or in perimenopause. - Decrease in size of the carpal tunnel.
For example after fractures with deformities or in case of deforming arthropaties which affect the form and the size of the tunnel, causing a narrowing.
N.B.: here there are some of the main working activities more at risk and for which carpal tunnel syndrome is recognized as an occupational diseases in many countries:- Shoes factory;
- Clothing factory;
- Meat/Fish processing;
- Fruit packing;
- Plastic processing;
- Manufacturing industry;
- Construction industry;
- Engineering and electronics industry.
What is the frequency (prevalence) of carpal tunnel syndrome?
How to diagnose a carpal tunnel syndrome?
The diagnose or diagnostic suspicion of CTS supposed on the base of symptoms, must be confirmed by an objective examination of the hand and by an electroneurographic-electromyographic examination (ENG-EMG).
- The objective examination of the hand is based on the inspection of the possible strength reduction on muscles or moreover on the inspection of the sensibility in the skin area (first three/four fingers) pertinent of median nerve. The doctor can improve this examination through some tests, that have proved to be useful for the purposes of the identification of a nerve compression. Main tests are the TINEL’S TEST (performed by flapping over the wrist area, in the carpal tunnel zone, with a percussion hammer; people affected by CTS generally feel a shock sensations which radiates on the fingers) and the PHALEN’S TEST (performed by having the patient maintain full wrist and finger extension for 1 minute: people affected by CTS generally feel the onset or the worsening of the tingling).
These tests and the objective examinations of the hand are very useful but they don’t give diagnostic certainties, so it is recommended, in any case, to confirm the suspicion with the electroneurographic examination. -

Electroneurographic (ENG) setting, usually sufficient to diagnose CTS.
The electroneurographic-electromyographic examination ENG-EMG: The electroneurography shows a slowing down of the nerve in transmitting bioelectrical impulses, in the zone of carpal tunnel. However sometimes, in order to have a clearer picture and to differentiate the CTS from nerve compressions in other points (for example in the cervical zone), it is necessary to proceed with a muscle investigation through the insertion of little needles (EMG). It must be remembered that some patients with a minimal form of damage nerve or with a sole disfunctional alteration of the nerve, could have a negative electroneurographic-electromyographic examination despite having a clear and intense symptomatology. Moreover the ENG-EMG examination, in addition to the diagnostic confirmation, allows to classify the disease according to the degree of nerve damage, through specific evaluation scales, that make easier to read the situation in which the nerve is.

Electromiographic (EMG) raw; it can be of help on CTS diagnose.
Does carpal tunnel syndrome get worse progressively?
Which is the CTS treatment?

Correct position on the computer, with arm, wrist and hand in a straight line.
Sometimes changing the work task, if possible, is sufficient to allieviate symptoms, in particularly avoiding the use of vibrating tools, or tools that compress on tunnel, and tryng to maintain the wrist aligned with the hand in using the keyboard (see fig.).
- Conservative treatment: it is recommended in all the mild and moderate forms of carpal tunnel syndrome, moreover it’s recommended in the temporary forms such as those related to pregnancy, or in other forms in which a surgical operation is contraindicated or also while waiting for the operation itself.
- Surgical treatment: is restricted to the more severe forms of CTS or in those forms that don’t react or react insufficiently to the conservative treatment.
Conservative protections proposed for carpal tunnel syndrome
- Physical therapy like ultrasound, iontophoresis and laser ( non-heating low frequency laser) to be performed on repeatable cycles.
- Wrist splinting with rigid braces: they block the wrist articulation preventing the flexion-extension. In this way they should prevent a higher compression of the nerve and also the worsening of symptoms during the night. This braces have been using for several years in countless versions; their efficacy is usually good, however they are not very tolerated because they are rigid, bulky and also they block the wrist. They’re particularly useful in CTS forms with evident and pronounced tendonitis at wrist.
-

Drug therapy is not usually effective or well tolerated.
Drugs: non steroidal anti-inflammatory (NSAIDs such as aspirin) and similars are generally considered as poorly effective. The steroidal anti-inflammatory (cortisone and similars) are surely more effective, but they present several contraindications and side effects, especially in the long run. Some molecules with anti-inflammatory or anti-edema action such as the “serratio peptidasi” are likely effective, particularly if associated with a conservative treatment. Drugs recommended for neuropathic pain are limited to few cases selected by the doctor.
- Local cortisone injections: they must be performed by expert medical staff. The technical execution of local injection must be accurated, otherwise it could lead to a irreversible fibrotic damage on the nerve.
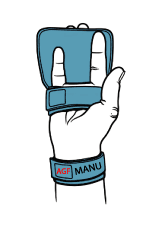
- INNOVATIVE SOFT DEVICE FOR THE HAND “MANU®“ (see dedicated FAQ).
Surgical treatment

Traditional open surgery.

Cutting surgery with endoscopic technique.
An opening is cut on the “roof” of carpal tunnel (transverse carpal ligament). There are different techniques:
- open carpal tunnel release, actuated through a classic incision on the palm;
- endoscopic carpal tunnel release; it involves one or two small incisions through which the nececessary instrumentation is introduced under indirect visual inspection.
In some cases specialists are not limited to section the transverse carpal ligament but they also remove one part. In other cases they try to remove the synovial fluid around the nerve (neurolysis). The purpose of these techniques is to improve results and to reduce the risk of recurrance, however not all agree on their validity. Some surgeons leave a little drainage catheter after the intervention. Anesthesia can be local or at the brachial plexus (under the armpit). Usually a tourniquet around the arm serve to limit postoperative bleeding. The stiches are generally removed after a week. A post-operative rehabilitation is often necessary. A rest of the operated hand is recommended, in variable times depending on the technique used (generally 3-4 weeks for open surgery). Traditional or open surgery is the most used in Italy; it could be performed with various techniques and incisions. Currently palmar mini-incision is being very used, especially from hand surgeons. Surgical treatment is generally efficient even if relapses or failures are not infrequent. Rare are complications such as: a) accidental section of variant branches, of a sensitive nerve branch at the base of the thumb or of a branch recurring on muscles of the same zone; b) anomalous cicatricial reactions; c) post-operative infections. The main causes of relapsing cases are the incomplete sectioning of the transeverse carpal ligament or its following reattachment. Surgical treatment of CTS, beyond the (rare) complications or relapses, constantly lead to a reduction of stability and strength in some hand functions (the so-called “pulley effect” of the transverse carpal ligament, that keep the flexor tendons of fingers anchored, goes missing).
What is MANU®?
MANU® reduces or even removes symptoms and improves the functionality of the hand.
MANU® has to be worn during the night for 1-3 months (cycles can be repeated if necessary).
MANU® doesn’t block the wrist and allows the index-thumb grip and also the thumb-little finger grip.



 (+39) 0861 372366
(+39) 0861 372366 info@agfmanu.com
info@agfmanu.com







